|
| Last belly pic. I took it Tues morning and didn’t know what the day had in store. |
Ever since I’ve been seen at the MFM and was feeling miserable with the extreme amount of fluid, my nurses would try to make me feel better by telling me this “horror story” of a woman who once got to a 60 AFI on her fluid measurement. Every week I was like “oh my gosh, you’re right, at least that’s not me.” Well, the day came. I was like at a 59.8. I heard the MFM doc in the hallway say, “This is ridiculous!” On the stress test, they could see that I was contracting every two minutes. So the nurse got permission to do a cervical check and I was at a 3. Between the cervical changes and the fluid, they took me to L&D for monitoring. I was desperate to go. I felt like I couldn’t breathe with the fluid and felt every contraction in my ribs. Basically the doctor said “we have a very low threshold for having a baby.” If I made any progress laboring on my own they were allowed to admit me to deliver- because of the complications and I was exactly 37 weeks.
Triage was miserable- a hour or two of not being able to get comfortable with the amount of fluid and trying to lay on a gurney. I started thinking- I might actually have this baby today. I regretted not eating before my appointment- I had planned to eat lunch after. And now I was laboring with low glucose. I lucked out and my nurse let me have graham crackers and apple juice and I felt so much better with a little bit of sugar. Especially since I did my insulin injection the night before.
I called a babysitter for the kids and texted Kevin to just be on standby in case I got admitted. I was so hopeful I would make progress because I was so desperate for them to break my water. Due to the pain, of course, but moreso I was afraid of it breaking away from the hospital due to the potential risks. Luckily, I progressed to a 4 within an hour and was admitted to have a baby!
With my other two kids, I never went into a regular labor on my own, and I was so thrilled my body was doing this on its own. No pitocin on board, and my contractions were nice and regular! They asked if I was okay to get the epidural before my water broke, in case of emergent surgery. I of course agreed because I did not want to be put under in an emergency if at all possible. If the situation was different, I definitely could have labored longer before asking for the epidural, but I knew things might change quickly as baby tried to adjust to the lack of all that fluid.
I dread getting epidurals because I have a congenital spinal fusion and they have always struggled to get it in the right place. I told the anesthesiologist when he came in that he’s going to have to place higher than he thinks due to the spinal malformation. I was hoping it would be a quick one or two tries, but it was actually the worst experience I’ve had with getting an epidural. He explained to me later that due to the fusion, the space they are looking for doesn’t really exist, but before he figured that out (and went much higher than he anticipated, like I said) he attempted over and over and over and over again. For an hour and a half I curled over, during contractions, hoping it would be over soon. I screamed every time it was in the wrong place and grated down those nerves. I tried so hard to be brave, but he struggled to get the local lidocaine to numb me very much. I kept asking for more lidocaine shots because it was excruciating- like being stabbed in the back.
Eventually I begged for a break, and he looked up CT images from like 2019 to help guide him with my anatomy. Every one of those “pops and clicks” as he described it, felt like a full on lumbar puncture. I was so exhausted with pain when we finally started to get some numbness in my feet. My back felt bruised and honestly stomped on.
 |
| All my epidural attempts |
I was excited to relax after my epidural, but I suddenly kept getting really nauseous and sick. Probably from the meds they pushed through my IV at the end of the epidural attempts to help me get through the continued attempts. I felt like I was passing out and throwing up at the same time. I broke out into a cold sweat. They ended up having to give me some IV meds to keep my blood pressure up because I kept dropping really low. When my pressure returned to normal I felt a million times better.
The doctor decided to do a controlled water break to try to slow down how fast all that fluid would drain. She fashioned a little tool with a small needle in it (instead of the usual tool they break your water with) to poke a very small hole in the sac and put pressure on that with her finger. Basically they didn’t want all of it to come flooding out and take any cord with it (cord prolapse is terrifying to me, let’s avoid that emergency). They didn’t want any baby limbs floating out with the “tidal wave” either. The doctor kept her finger on that membrane as long as she could until everything had ripped and the fluid had drained. I could not believe the number of towels soaked during this procedure. When it was all done, I seriously did not even feel pregnant any more due to the pressure relief. I was so happy that my water was broken in a controlled environment. The anxiety of it breaking somewhere else resulting in major complications was finally gone.
Pretty quickly after my water broke, Ivy’s heart rate started dropping. They repositioned me to see if we could move any pressure off the cord, but nothing changed. Afterwards, they asked permission to place an internal monitor to make sure what we were seeing was accurate. It was. After that, with her stress still evident, they started infusing saline back in to the uterus, to see if that would help her adjust to such a huge and sudden change in pressure from a large amount of fluid being gone.
I was still at 4cm at this point, and the doctor came to talk to me. She said she was concerned that Ivy wasn’t tolerating labor and that I still had a long way to go. She said if I was at a 9 she would be more comfortable trying to push through to the end, but she was worried about a possible placental abruption (when the placenta detaches too early) due to the uterus shrinking so rapidly after a massive amount of fluid draining. She said we were stable at this point, but I should consider how I felt about a c-section. I told her I understood everything she said and I would rather go before it was a true emergency because if it’s an abruption I don’t want my baby going without oxygen.
And off we went to the OR. (Spoiler alert: I did have a placental abruption due to the quick and major change in size of the uterus. About 30% had detached. I’m so thankful I started going into full labor AT the hospital. I’m relieved we were able to do a controlled water break. If my water broke at home on its own, with so much extra fluid, outcomes could have been very different.)
I have always been afraid of a C-section. Not because I’m afraid of surgery, but because my body metabolizes certain drugs really fast and I struggle with pain relief and getting numb. I have woken up during scopes, been rescheduled by the dentist after they max out on novocaine without success, had conscious sedation fail during eye surgery, and the list goes on! I’ve had too many experiences of suddenly feeling sharp, searing pain when I’m supposed to be numb. I tell doctors to “dose me like a redhead!”
Luckily (or not) the anesthesiologist had experienced this with me firsthand when trying to numb me and place my epidural. He said he was planning to give me everything he could safely in surgery.
When I was on the table, I just looked at Kevin and felt the panic surge when they put the blue drape up. I had been told before a spinal makes it so you “can’t even feel that you have legs”; I still felt like I could perhaps move my legs and feet. I looked at Kevin and just said over and over through tears, “I’m scared, I’m scared.” At that point however, Ivy’s heart rate was down to 90 and my doctor said “Okay, I don’t like that, let’s go now.” That helped me focus, we needed to get her out. I’m glad we didn’t wait. In spite of how awful it was to get the epidural placed- it worked. I didn’t feel the sharp pain of surgery. I did feel the “pressure” of birthing her, when a big tall doctor got up on a stool and put his whole weight on my abdomen to help push her out.
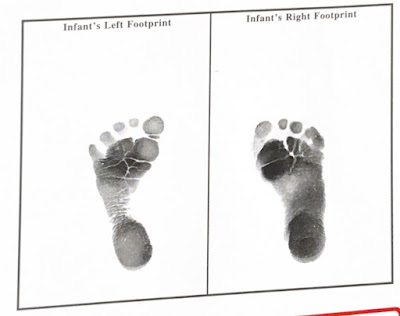
Ivy Laine Hanni
Born 8:29pm at 37 weeks
7lbs 11oz
19.5 inches
I don’t remember a lot about after she was born, because that’s when they push the bigger drugs to finish surgery. I do remember telling Kevin that Ivy was beautiful! They took my tubes out before closing as I had requested in advance. I know we are done having children, and I’m so done after 10 pregnancies in total. It’s still a weird kind of sadness (especially weird to have mixed feelings since Kevin already had a vasectomy before she was born!)
I remember asking where Ivy was as they were finishing surgery. Kevin reassured me that she was being checked out by the team and getting some respiratory support. I wasn’t too worried about her needing some CPAP at the time (pretty common) but maybe part of it was the drugs, because I don’t actually remember her crying and it seems that would have worried me. Kevin told me later she didn’t ever have a strong cry after birth.
 |
| Kev’s first look. I do not like how floppy she looks here- sets off all the alarm bells |
 |
| 1-2 seconds later. Thank you to her awesome medical team |
At some point I was told that Ivy was being admitted to the NICU. She was requiring help past the 3 hours of “transition” they give them. I was sad that I still hadn’t met her, but they told me they could take me down to the NICU. She was on CPAP so she wasn’t able to eat yet. I was told I could start pumping and they could tube feed the colostrum the next day. She was on IV clears in the meantime. They admitted her under the diagnosis of respiratory distress syndrome and told me she would be on IV antibiotics for a few days to rule out infection as a cause.
 |
| Meeting my babe |
It was the weirdest feeling not being with my baby, she almost didn’t feel like mine. I was in a unit with lots of moms and babies, and I was just in a room without a baby. Her eyes were so swollen and with the CPAP and tubes, etc I could barely make out what she looked like.
 |
| Two girls looking a little beat up after the birthing experience. Matching swollen eyes. |
Wednesday- My blood pressure had been low and I was feeling sick from it, so they drew some labs. The doctor came in and told me I was borderline for needing a blood transfusion (looking at the pictures now, that makes sense- I looked like a vampire). I ended up getting an iron infusion to start and then they decided against the blood since I started doing a little better.
I found out that between my blood clotting risks and having surgery, I have to do lovenox injections for 6 weeks. I was so excited to quit the insulin injections- but now I am switching to a way more painful daily shot.
I’m sad that I don’t really remember the kids meeting Ivy. I kind of do, but it’s more like snippets of a dream than a memory. I remember some family coming to meet her, but just pieces. I wasn’t sure it really happened. I felt really vulnerable later like- what did I say and do when people came to visit?! Those surgery drugs all caught up to me. Lactation came to try to talk to me and do some education and I fell asleep sitting up TWICE while talking to the woman. I feel bad about that…but I’m sure it’s not the first time it’s happened.
 |
| Pretty baby. Her skin is really red here from polycythemia- which can happen with gestational diabetes. It didn’t cause any major issues. |
Ivy was only tube feeding at the moment due to respiratory distress, which made me really sad that I couldn’t try to breastfeed her. She really liked when I would get to the NICU and do skin to skin with her. My hopes were that she could go from bubble CPAP to high flow oxygen, to try to help her discomfort and swelling (and so she could maybe nonnutritive breastfeed during the tube feed.) But she wasn’t stable enough. We also found out she has a tongue tie also.
 |
Trialing high-flow oxygen
|
 |
| ivy laine <3 |
Thursday
My poor girl had to go back on bubble CPAP, she had increased work of breathing and her chest X-ray was worse. I didn’t expect this with a 37 week gestation baby, there are babies way younger than her on much lower respiratory support. I thought maybe she would need a low flow nasal cannula for a day or two. I couldn’t understand the full picture of what the problem is.
Friday
I’m miserable watching how restless she is. I want her to know who I am. I hate that she’s 4 days old and has never attempted to breastfeed (you have to be able to breathe for that). We have been trying skin to skin more, she really seems to calm doing that with me. Kevin gave her a really nice father’s blessing.
While the medical team expects that inflammation and fluid are to blame for her respiratory problems, they aren’t entirely sure why it’s happened. They are unsure if it is related to the polyhydramnios. Ivy hates the CPAP but she’s worn out from working so hard to breathe.
I know things could be so much worse, but they are discharging me tomorrow. To leave my baby at the hospital and go home feels criminal. I’ve watched lots of other families come and go with their babies and I wish that was our situation. I’m just happy she’s alive. She’s here. We’ll be okay.
I will do a future post about our NICU journey <3