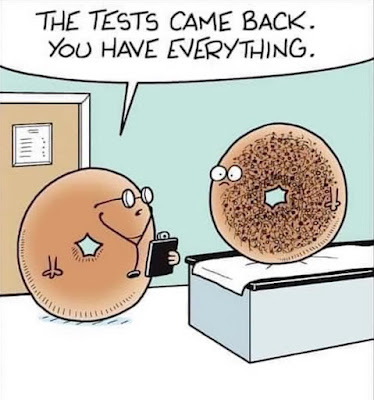
If you’ve been reading my blog for the past ten years, you‘ll appreciate my similarities to the bagel.
When I concluded my last blog post, I was looking forward to finishing up treatment and finally moving towards a resolution of our fertility journey. When I finished the two weeks of Cipro and Flagyl together I felt like I won a gold medal. I was so relieved to be rid of those meds and braced myself to endure the repeat biopsy, it would all be worth it because the end was in sight. I just had to wait for the proper cycle timing for the biopsy appointment.
I asked my doctor’s opinion regarding my full time position working nights as I’ve been concerned about harm to a potential pregnancy. I’ve read limited research about night shifts (obviously) messing with your circadian rhythms and hormone regulation, potentially leading to an increased risk of miscarriage. I wanted my doctor’s advice to navigate this. Clearly, many people work nights all the way through their pregnancy and have perfect outcomes. I just always feel like I’m the outlier.
My doctor did not feel that it would be a major risk to a pregnancy to continue working nights despite my complicated history. It was a huge sigh of relief to hear I didn’t need to change my schedule, but the relief was short lived. I still felt worried about it. I know of at least 3 coworkers who have miscarried while at work during the night. It’s empirical evidence and probably not clinically significant, but my anxiety wins in this situation. I really feel the need to reduce the stress on my body. It’s no secret that working 12-13 hour shifts, 3-5 nights in a week, is hard on the body.
Jack and Aidia are nearly out of school for the summer, and as I was trying to determine how to balance work and childcare, I decided it was best to reduce my hours to part time temporarily. While it reduces the cost of childcare, it’s still a leap of faith to drop to part time. I hope by the end of the summer we will be out of this period of uncertainty. By the fall, I imagine we’ll have a better understanding of our fertility situation and can make the best decision about work schedules.
We are in the exhausting limbo phase. I feel restless and impatient. We haven’t even been trying to conceive yet, and I’m feeling the strain of 6 months of testing with the fertility clinic. I think it feels heavier more quickly because it’s compounded with the past decade. It just feels like this part is taking forever. I either want to be pregnant, or endure the worst and know that the door is closed for us. Trying to plan a life around “what ifs” is so mentally exhausting. My kids are soon headed into 8th grade and 2nd grade. I’m in a totally different phase of parenting and need to know if I’m going to be caring for a baby and a teenager simultaneously, plus one in the middle.
Thankfully, in the middle of all this cognitive dissonance and disequilibrium, Kevin and I were able to go away for a weekend as part of a work conference. It was absolutely the best thing and I needed the breath of fresh air. We jam packed as many activities as we could and it was a reminder of what it feels like to actually be alive; not so bogged down with daily responsibilities and parenting. We even did a zip line, which was scary but I finally crossed something off my bucket list!
The trip was a reminder to me that there is lots of joy to be found in life, whether we get a final miracle baby or not. All hope is not lost, and there is lots to live for and look forward to. We have some summer shows, concerts, and family reunions planned. We’re even taking the kids on a little vacation to Vegas. I’m happy to find what life looks like solidly into our 30s. It’s so much better than our 20s. Aging is fantastic. The “just in case” aspect of planning months in the future is still hard. I worry about “what if I’m going through a loss in x amounts of months.” But, it’s wonderful to feel like I’m actually living my life. I don’t want to wait on it anymore.
Before the trip, I happened to see a job listing for a PRN position for a RN at Maternal Fetal Medicine. Immediately, I was excited about the prospect, but didn’t submit a resume because the stress of picking up another part time job seemed like too much. More so, I worried about my own personal triggers while trying to care of others. Some of the most traumatic and sensitive experiences of my life have taken place in clinics like an MFM office. But the job stayed in my mind the whole weekend away. Perhaps my experiences would truly serve me in the ability to be a compassionate and empathetic nurse. Since I couldn’t stop thinking about it, I applied when we returned home. Turns out they had already filled the position so I didn’t even interview, but it still felt like a win. Despite my mixed feelings of fear at the idea of working in a triggering environment, I was equally excited about the possibility of serving women in a population I’ve been a part of. I proved to myself that I can still put myself out there, in the speciality of my interest. I can keep progressing while carrying all my complicated feelings with me.
The time came for the repeat biopsy. I wasn’t looking forward to the procedure but I was ready to move on from these tests. Doing the repeat biopsy was really just for my peace of mind, since the treatment I completed is so effective.
Thankfully the repeat biopsy was much more tolerable than the previous one. Maybe they didn’t remove a polyp in the process this time. I also thought if the endometritis had cleared up, maybe the tissue would be less sensitive. I was very hopeful.
When my results came in, I was ready to tie a nice little bow on the testing phase of our fertility journey. I was so excited to move on and possibly conceive a healthy baby. The worst surprise. My biopsy came back positive again. The clinic was so sure treatment would work, they said I didn’t need to do a repeat biopsy. The studies clearly show that most cases of chronic endometritis are cured with antibiotics. Again, I’m the outlier. I’m so glad I listened to my gut about repeating the test. Still, I felt so shocked about the result and really sad.
Upon seeing the result, one of my first thoughts came with a jolt. I wondered, “does this mean I need ANOTHER biopsy?” That would be a grand total of 4, 3 of them being right in a row. It hurts my womb just to think about it. I really don’t want to go through it again. But could I risk NOT getting another biopsy after realizing how stubborn this infection is? Probably not.
I’m wearing out. I could not even imagine doing more antibiotics. I’m so exhausted by all of this. But it’s not even like I can just say “ok we’re just going to be done, it’s too much,” because I can’t just walk around with a lingering infection forever. I started considering the idea of a D&C to try and cure this. Just scrape me out like a pumpkin. It’s fine. Here’s a link to a study published last year about using a surgical approach in the treatment of chronic endometritis.
However, my doctor decided on the treatment that I initially did in 2019: doxycycline twice a day for a month. I'm so overwhelmed. Another MONTH of antibiotic therapy is my nightmare right now. I wish I could just get these meds infused, I am not going to have a stomach left. Plus, fun fact about doxycycline, you are supposed to avoid the sun as side effects include photosensitivity; even a small/normal amount of sun exposure could potentially have pretty bad outcomes. Time to break out the hard core SPF.
The med bottle may as well have read, “Please do not enjoy spring while ingesting this poison.”
Perhaps unironically, this was the same day I started finding my first grey hairs while fixing my hair for work. How did so many pop up all at once?!
I reduced my vitamins for the time being and added more probiotics and lysine to counteract the mouth sores and tummy upset from the antibiotic. It’s still hella pills though.
Fortunately I have a depressing new Taylor Swift album to bask in this week, which is helping a lot.
Fortunately, I have a really great therapist and we’ve been doing a lot of work to help me get through these challenges in a healthy way. I think many people fail to realize that with recurrent loss, all these desperate feelings and disappointments are compounded with all your previous hardships experienced in years before. Small bits of bad news can sometimes feel crushing and you can slip back into horrific moments of loss that came before.
We’ve been working on “radical acceptance” which is a concept I had somewhat been finding on my own, without the official name. A lot of therapy principles we work with stem from Daoism and Buddhism. When you remove some of the spirituality, these Eastern concepts morph into very effective Western (clinically-proven) therapy techniques. I love the wisdom found in Eastern dogmas.
Basically, radical acceptance is a way to prevent pain from turning into suffering. It’s recognizing that reality includes pain, and accepting it anyway. It’s understanding that some things will remain out of your control. It’s accepting emotions and circumstances that may not be changeable. Embrace (and don’t avoid/ignore) what you can’t change.
In my mind, I go to the Beatles, who summed it up so beautifully. Let it be.
“Parts work” has been extremely effective for me. I try to acknowledge each little “part” of me and appreciate its purpose and how an emotion may be trying to help or protect me. “No Bad Parts” is a great book if you are interested in learning more about this model.
I learned in therapy that confusion and clarity are two sides of the same coin. If we allow ourselves to sit with the uncomfortable, it can become clarity.
All of this is not to say that things are easy. They often feel heavy, depressing, and I get restless. Not to mention the physical effects from treatments. But therapy like this is getting me through. It helps.
In what felt like that moment of clarity, I applied for my dream job. A full time NICU position at Primary Children’s Hospital. I was trying to build experience little by little before ever applying, and I thought, screw it, can’t hurt to go for the gold. I have spent the past couple years working in what is essentially a step-down NICU. I mean, I’m not pregnant and my uterus isn’t getting better. I could be months away from even trying to conceive. I don’t want to put off an opportunity for a “what if.” If we miraculously conceive a healthy baby, I will cross that bridge when I get there.
It’s a big career goal of mine to get my neonatal intensive care certification. It takes a couple years of working in the NICU setting and then you can sit for the exam to get that beautiful RNC-NIC credential.
It’s a long shot at a competitive position. I’m sure it depends on what type of candidates apply, especially if there are potential internal hires. I don’t know how I would work out the full time with rotating days and nights, yet. But I would be stupid not to try. Opportunities come and go, and I’m proud of myself just for giving it my best shot.